Safety Information
Safety Information
Prescribing Information [External link]
Please refer to the Summary of Product Characteristics for full prescribing information.
An established safety profile1
Clinical studies
In healthy children aged 12 months to 12 years (N=5185) given 1 dose of VARIVAX, the most frequent adverse events reported in temporal association with vaccination were:1
| Frequency | Adverse event(s) |
|---|---|
| Very common (≥1/10) | ● Fever |
| Common (≥1/100, <1/10) | ● Upper respiratory infection ● Rash ● Maculopapular rash ● Varicella-like rash (generalised median 5 lesions) ● Injection site erythema ● Pain/tenderness/soreness ● Swelling ● Varicella-like rash (injection site median 2 lesions) ● Irritability |
The following serious adverse events temporally associated with the vaccination were reported in individuals 12 months to 12 years of age, given the vaccine (≥3 months apart): diarrhoea, febrile seizure, fever, post-infectious arthritis and vomiting.
The rates of systemic clinical adverse events after a second dose of VARIVAX were generally similar to, or lower than, those seen with the first dose. The rates of injection-site reactions (primarily erythema and swelling) were higher after a second dose.
Please refer to the Summary of Product Characteristics for further details on less frequent adverse events reported in people who received VARIVAX.
VARIVAX contraindications1
- History of hypersensitivity to any varicella vaccine, to any of the excipients or neomycin (which may be present as trace residues)
- Blood dyscrasias, leukaemia, lymphomas of any type, or other malignant neoplasms affecting the hemic and lymphatic systems
- Individuals receiving immunosuppressive therapy (including high doses of corticosteroids)
- Severe humoral or cellular (primary or acquired) immunodeficiency, e.g. severe combined immunodeficiency, agammaglobulinaemia and AIDS or symptomatic HIV infection or an age- specific CD4+ T-lymphocyte percentage in children below 12 months: CD4+ <25%; children between 12-35 months: CD4+ <20%; children between 36-59 months: CD4+ <15%
- Individuals with a family history of congenital or hereditary immunodeficiency, unless the immune competence of the potential vaccine recipient is demonstrated
- Active untreated tuberculosis
- Any illness with fever >38.5°C; however, low-grade fever itself is not a contraindication to vaccination
- Pregnancy. Furthermore, pregnancy should be avoided for 1 month following vaccination
Special warnings and precautions for use1
- As with all injectable vaccines, appropriate medical treatment and supervision should always be readily available in case of a rare anaphylactic reaction following the administration of the vaccine.
- As for other vaccines, there is the possibility of hypersensitivity reactions, not only to the active principle, but also to any of the excipients of the vaccine, including neomycin (which may be present as a trace residue).
- As with other vaccines, VARIVAX does not completely protect all individuals from naturally acquired varicella. Clinical trials have only assessed efficacy beginning 6 weeks after a single dose in healthy individuals up to 12 years of age or 6 weeks after the second dose in older subjects.
- Vaccination may be considered in patients with selected immune deficiencies where the benefits outweigh the risks (e.g., asymptomatic HIV subjects, IgG subclass deficiencies, congenital neutropenia, chronic granulomatous disease, and complement deficiency diseases).
- Immunocompromised patients who have no contraindication for this vaccination may not respond as well as immunocompetent subjects; therefore, some of these patients may acquire varicella in case of contact, despite appropriate vaccine administration. These patients should be monitored carefully for signs of varicella.
- Vaccine recipients should avoid use of salicylates for 6 weeks after vaccination.
- Transmission of varicella vaccine virus (Oka/Merck strain) resulting in varicella infection including disseminated disease may rarely occur between vaccine recipients (who develop or do not develop a varicella-like rash) and contacts susceptible to varicella including healthy as well as high-risk individuals.
- Therefore, vaccine recipients should attempt to avoid, whenever possible, close association with susceptible high-risk individuals for up to 6 weeks following vaccination. In circumstances where contact with high-risk individuals is unavoidable, before vaccination, the potential risk of transmission of the vaccine virus should be weighed against the risk of acquiring and transmitting the wild-type varicella virus.
- Susceptible high-risk individuals include: immunocompromised individuals, pregnant women without documented positive history of chickenpox or laboratory evidence of prior infection, new-borns of mothers without documented positive history of chickenpox or laboratory evidence of prior infection.
Interaction with other medicinal products and other forms
of interaction1
VARIVAX must not be mixed with any other vaccine or other medicinal product in the same syringe. Other injectable vaccines or other medicinal products must be given as separate injections and at different body sites.
Concomitant administration with other vaccines
VARIVAX has been administered to toddlers at the same time as, but at a different injection site from, a combined measles, mumps, and rubella vaccine, Haemophilus influenzae type b conjugate vaccine, hepatitis B vaccine, diphtheria/tetanus/whole-cell pertussis vaccine, and oral polio virus vaccine. There was no evidence of a clinically relevant difference in the immune responses to any of the antigens when co-administered with VARIVAX. If VARIVAX is not given concomitantly with measles, mumps, and rubella virus vaccine live, a 1-month interval between the 2 live virus vaccines should be observed. Concurrent administration of VARIVAX and tetravalent, pentavalent or hexavalent (diphtheria, tetanus, and acellular pertussis [DTaP])-based vaccines has not been evaluated. Vaccination should be deferred for at least 5 months following blood or plasma transfusions, or administration of normal human immune globulin or varicella zoster immune globulin (VZIG). Administration of varicella zoster virus antibody-containing blood products, including VZIG or other immune globulin preparations, within 1 month following a dose of VARIVAX may reduce the immune response to the vaccine and hence reduce its protective efficacy. Therefore, administration of any of these products should be avoided within 1 month after a dose of VARIVAX unless considered to be essential. Vaccine recipients should avoid use of salicylates for 6 weeks after vaccination with VARIVAX as Reye syndrome has been reported following use of salicylates during wild-type varicella infection.
Pregnancy and Lactation1
Pregnancy
Pregnant women should not be vaccinated with VARIVAX. Studies have not been conducted with VARIVAX in pregnant women. However, foetal damage has not been documented when varicella vaccines have been given to pregnant women. It is not known whether VARIVAX can cause foetal harm when administered to a pregnant woman or can affect reproduction capacity. Pregnancy should be avoided for 1 month following vaccination. Women who intend to become pregnant should be advised to delay.
Breastfeeding
Due to the theoretical risk of transmission of the vaccine viral strain from mother to infant, VARIVAX is not generally recommended for breastfeeding mothers.
Vaccination of exposed women with negative history of varicella or known to be seronegative to varicella should be assessed on an individual basis.
References
- VARIVAX Summary of Product Characteristics. Available at: https://www.medicines.org.uk/emc/product/5582/smpc
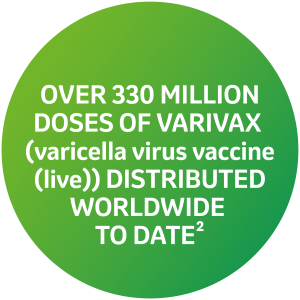
- MSD Data on File. Vaccine Products Global Doses Distributed Memo Q2/2024.
Supporting documentation
Prescribing Information
By clicking the link above you will leave the MSD Connect website and be taken to the emc PI portal website
